| What is Mukhyamantri Amrutum (MA) Yojana? Mukhyamantri Amrutum (MA) Yojana is a state-sponsored health insurance scheme launched in 2012 by then Chief Minister Narendra Modi to provide free cashless medical and surgical treatment to economically vulnerable families in Gujarat. Initially designed as a state-only program, it was later aligned with the Pradhan Mantri Jan Aarogya Yojana (PMJAY), creating the co-branded PMJAY-MA Yojana. |
Healthcare costs can be a significant burden, especially for low-income families facing critical illnesses. Recognising this challenge, the Gujarat government introduced the Mukhyamantri Amrutum (MA) Yojana to ensure that vulnerable households have access to quality medical care without financial hardship. Over the years, the scheme has evolved into a robust health protection programme through integration with national initiatives.
In 2023, coverage was enhanced to ₹10 lakh per family per year, with benefits now portable nationwide across empanelled hospitals. As of September 2025, the scheme has settled 51.27 lakh hospitalizations, paying out ₹13,946.53 crore to hospitals, making Gujarat the second-highest spender under AB-PMJAY nationally.
By the end, you’ll get a complete guide to the Mukhyamantri Amrutum Yojana — including its features, eligibility criteria, benefits, enrollment process, and frequently asked questions.
Looking for comprehensive health coverage beyond MA Yojana? Ditto helps you compare the best health insurance plans so you can choose what’s right for you. Book a free consultation today.
Features and Benefits of Mukhyamantri Amrutum Yojana
The Mukhyamantri Amrutum (MA) Yojana was introduced to protect Below Poverty Line (BPL) families in Gujarat from the burden of catastrophic medical expenses. With the PMJAY-MA integration, it now extends wider coverage and portability.
Here are the key features and benefits that make this scheme a vital healthcare safety net for eligible families:
- Provides cashless health coverage up to ₹5 lakh annually per family (₹10 lakh after PMJAY-MA integration in Gujarat).
- Beneficiaries can access treatment at any empanelled public or private hospital.
- Covers a wide range of critical illnesses and high-cost surgeries, including cancer, cardiac, kidney, and accident-related care.
- Includes 2,400+ benefit packages across cardiovascular, neurosurgery, oncology, burns, renal care, neonatal diseases, and poly-trauma. If you want to check the rates offered to empanelled hospitals for these treatments, you can check here.
- Offers surgical, medical, and emergency treatments without out-of-pocket expense for eligible families.
- Coverage includes eye surgeries, ENT treatments, joint replacements, and transplants without any pre-existing disease waiting period. This makes it a highly advantageous plan as compared to private retail health insurance plans, which cover PEDs only after 1-3 years unless reduced with add-ons.
- Provides pre- and post-hospitalisation expenses along with the treatment.
- Transport allowance available for patients needing to travel to hospitals up to ₹300 per visit.
- Co-branded PMJAY-MA card ensures seamless access to benefits under both central and state schemes.
- No premium or registration fee is charged from beneficiaries.
In short, the MA Yojana serves as a lifeline for vulnerable households in Gujarat.
Eligibility for Mukhyamantri Amrutum (MA) Yojana
The Mukhyamantri Amrutum (MA) Yojana ensures below poverty line families have access to quality medical care without financial stress. For enrollment, all family members are required to be physically present.
In addition, a separate MA Vatsalya Yojana covers families just above the poverty line under certain criteria. This structure ensures that the scheme covers not only the poorest families but also vulnerable groups slightly above the poverty line, safeguarding their healthcare needs.
Here’s a quick look at who qualifies for the Mukhyamantri Amrutum (MA) Yojana:
- Families listed in the BPL list by the Gujarat State Government are eligible under MA Yojana.
- Families with an annual income up to ₹4,00,000/- can apply under MA Vatsalya Yojana.
- Accredited Social Health Activist (ASHA) workers and their families are eligible.
- Families of accredited journalists/reporters can avail benefits.
- Class 3 and Class 4 employees working on fixed payroll with the Gujarat Government are covered.
- Senior citizens with a total family annual income of up to ₹6,00,000/- are eligible.
Documents Required to Apply for MA Scheme
To enroll under the Mukhyamantri Amrutum (MA) Yojana, applicants must provide valid documents for verification. These ensure eligibility and smooth issuance of the MA/PMJAY-MA card. The required documents include:
- Proof of income (e.g., income certificate issued by competent authority).
- Government-issued ID proof (such as Aadhaar card, voter ID, or PAN card).
- Proof of residence (ration card, electricity bill, or any utility bill).
- Category-specific supporting documents for groups like widows, orphans, senior citizens, etc.
Submitting accurate and up-to-date documents is essential to successfully complete enrollment and avail cashless healthcare benefits under the scheme.
How to Enroll under MA Card Yojana?
The enrollment process for the Mukhyamantri Amrutum (MA) Yojana is conducted offline at designated centers across Gujarat. Eligible families can follow these steps to get their MA/PMJAY-MA card:
1) Visit a Registration Center
a. Enrollment can be done at civil hospitals, taluka-level centers, or Community Service Centers (CSCs).
b. Other authorized centers include E-Gram centers, UTI-ITSL centers, and nCode Agency centers.
2) Provide Required Documents
- Proof of income (income certificate).
- Government-issued ID proof (Aadhaar card, voter ID, etc.).
- Proof of residence (ration card, utility bills, etc.).
- Supporting documents for specific groups like widows, orphans, or senior citizens.
3) Verification and Card Issuance
- Submitted documents are verified by officials.
- Once approved, beneficiaries receive a co-branded PMJAY-MA smart card for cashless treatment.
By completing this simple enrollment process, eligible families can access free medical care across Gujarat and at empanelled hospitals nationwide.
Why Should You Approach Ditto for Your Health Insurance?
At Ditto, we’ve assisted over 7,00,000 customers with choosing the right insurance policy. Why customers like Abhinav below love us:
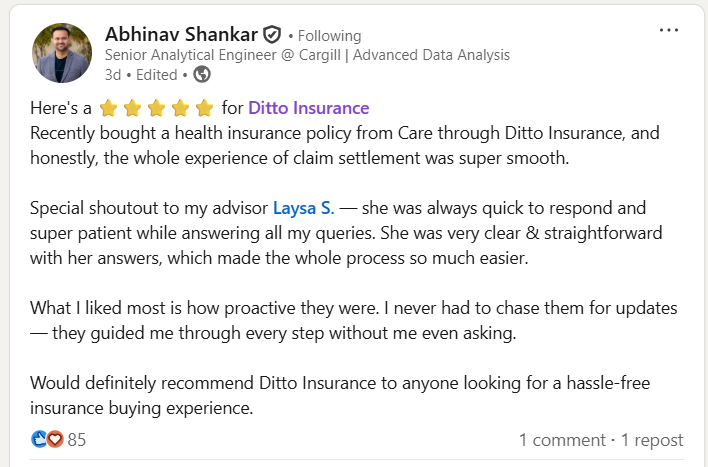
✅No-Spam & No Salesmen
✅Rated 4.9/5 on Google Reviews by 15,000+ happy customers
✅Backed by Zerodha
✅100% Free Consultation
You can book a FREE consultation. Slots are running out, so make sure you book a call now!
Conclusion
The Mukhyamantri Amrutum (MA) Yojana, now integrated with PMJAY, offers comprehensive financial protection to Gujarat’s vulnerable families. With free cashless coverage, a wide hospital network, and portability across India, it ensures that critical healthcare is accessible without financial strain.
For those who are not eligible or prefer higher coverage, a choice of premium hospitals and doctors, private health insurance remains a reliable way to secure similar protection.
Looking for personalised health coverage advice? Book a free consultation with Ditto today and explore options that go beyond government schemes to give you complete peace of mind.
FAQs
How to claim benefits under Mukhyamantri Amrutum (MA) Yojana?
You can claim benefits by presenting your MA/PMJAY-MA smart card at any empanelled hospital. The treatment is completely cashless, and the hospital directly settles bills with the scheme authorities.
Are there any costs involved in enrolling into Mukhyamantri Amrutum (MA) Yojana?
No, there are no enrollment or premium costs. The scheme is fully funded by the Gujarat government, ensuring free access for eligible families.
How many family members are covered under the MA Yojana?
The scheme provides coverage to the entire registered family unit, as per the BPL or MA Vatsalya records.
Can MA Yojana benefits be used outside Gujarat?
Yes, after integration with PMJAY, beneficiaries can avail cashless treatment at empanelled hospitals across India using the co-branded card.
What types of treatments are covered under MA Yojana?
The scheme covers critical and high-cost treatments, including cancer care, cardiac surgeries, kidney transplants, neonatal diseases, trauma, and more than 2,400 medical packages
What are the hospital empanellment guidelines for the Mukhyamantri Amrutum (MA) Yojana?
You can check the hospital empanellment guidelines for the Mukhyamantri Amrutum (MA) Yojana here.
Where can I access government provided FAQs for the Mukhyamantri Amrutum (MA) Yojana?
Last updated on:










