| What is an Indemnity Health Insurance Plan? Indemnity Health Insurance plans provide coverage for actual hospital expenses. Instead of paying a fixed amount, the insurer covers costs like room rent, surgery, ICU charges, and medicines, up to your sum insured. |
Whenever you hear someone talk about health insurance, they’re usually referring to an indemnity health insurance plan, often called a comprehensive or mediclaim policy. At Ditto, we’ve helped thousands of Indians navigate health insurance every month. For this guide, we’ve drawn insights from IRDAI regulations, real policy documents, and our experience assisting customers with claims.
By the end, you’ll know exactly what an indemnity health insurance plan means, how it works, and the best way to choose the right plan for your needs.
Not sure which indemnity plan fits you? Get expert help from Ditto – no spam, no salesmen, just honest advice.
What is covered and not covered under Indemnity Health Insurance?
Indemnity health insurance plans usually provide coverage for:
- In-patient hospitalisation – Covers expenses when you are admitted to the hospital for more than 24 hours, including treatment, nursing, and doctor’s fees.
- Room rent – Takes care of daily room charges, whether in a shared ward, private, or deluxe room (as per policy terms).
- Surgeries and procedures – Pays for surgical expenses, operation theatre charges, anesthesia, and recovery care.
- Accidents and emergency care – Covers hospitalisation due to accidents or emergencies, protecting you from sudden expenses.
- Pre- and post-hospitalisation – Reimburses medical costs like diagnostics, consultations, and medicines incurred before admission and after discharge (usually 30–90 days before and 60–180 days after).
- Domiciliary hospitalisation – Provides cover if you need treatment at home because hospitalisation isn’t possible.
- Daycare treatments – Includes procedures such as dialysis, cataract surgery, or chemotherapy that don’t require 24-hour admission.
- AYUSH treatments – Covers alternative systems of medicine like Ayurveda, Yoga, Unani, Siddha, and Homeopathy.
- Annual health check-ups – Preventive health check-ups are included after a specific waiting period, which covers routine tests such as blood sugar, cholesterol, Blood pressure, and BMI readings, among others.
- OPD treatments (in some plans) – Covers doctor consultations, diagnostics, and medicines without the need for hospitalisation.
- Maternity costs (via riders/add-ons) – Extends coverage to delivery expenses, newborn care, and related medical needs if opted as an add-on.
Standard Exclusions in Indemnity Health Insurance
- Initial waiting period – No claims (except accidents) are allowed within the first 30 days of buying the policy.
- Pre-existing diseases (PEDs) – Covered only after a waiting period, usually up to 3 years.
- Specific treatments – Certain conditions like hernia, piles, or joint replacement, may have their own waiting periods of up to 2 years.
- Cosmetic or plastic surgery – Excluded unless required due to an accident or medical necessity.
- Self-inflicted injuries – Injuries caused by intentional harm, suicide attempts, or substance abuse.
- Professional extreme sports – Injuries sustained while participating in hazardous or adventure sports professionally are not covered.
- Dental surgeries – Unless arising from an accident or if specifically included in the policy.
- Ophthalmological treatments – Refractive error correction (like LASIK) is excluded if below 7.5 diopters.
- Gender affirmation surgeries – Usually excluded unless the insurer explicitly provides coverage.
- Non-medical expenses – Items like food, admission fees, or unlisted consumables are not reimbursed.
- Unproven or experimental treatments – Procedures not approved by medical authorities are excluded.
Note: The exclusions listed above are for illustrative purposes only. Always check the policy wording of your specific plan to know the exact coverage and exclusions provided by your insurer.
How does Indemnity Health Insurance Work?
Indemnity health insurance works based on the principle of indemnity in insurance, which dictates that a policyholder should be compensated for the actual financial loss they suffer, not to make a profit from the loss.
The goal is to restore the insured to their exact financial position before the loss occurred. It may sound harsh, but insurers do this to deter people from misusing their policy benefits.
This principle applies to most health, property and liability insurance but not typically to life insurance, where the value of human life cannot be assigned a fixed monetary value.
Indemnity Health Insurers That Make Ditto’s Cut
| Before we discuss the list, here’s how we decide what plans to feature. At Ditto, every health insurance plan and insurer undergoes our six-point evaluation framework. It doesn’t mean these are the only good plans/insurers, but that they stand out after being scored across all six pillars. You can learn more about how we evaluate health insurance plans here. |
| Health Insurer | AVG. CSR (2022-25) | AVG. Complaints (2022-25) | AVG. ICR (2021-24) | Network Hospitals | AVG. GWP/ Annual Business (2022-25) |
|---|---|---|---|---|---|
| HDFC ERGO | 97 | 9 | 86 | 13000+ | ₹6178 crores |
| Care | 93 | 42 | 59 | 11400+ | ₹6775 crores |
| Aditya Birla | 96 | 19 | 68 | 12000+ | ₹3290 crores |
| Industry Mean/Median | 91.22 (mean) | 16.90 (median) |
82.62 (median) |
10000+ (industry norm) |
₹1944 crores |
Premiums for Ditto’s Recommended Indemnity Health Insurance Plans
| Profiles | Premiums |
|---|---|
| (Individual Plan): Age 25 |
₹10149- ₹14592 |
| (Family Floater, 2A): Ages (31, 32) | ₹16,299- ₹22,272 |
| (Family Floater, 2A 1C): Ages (35, 34, 5) | ₹21,478- ₹27,222 |
| (Family Floater, 2A): Ages (62, 63) | ₹66,505- ₹81,829 |
Note: The premiums above are for a ₹15 lakh sum insured, with the proposer residing in Delhi – 110010. The amounts are inclusive of essential riders/add-ons (such as consumables coverage, cumulative bonus, etc.). In addition, the ranges provided are for the flagship health insurance plans from the insurers mentioned in the metrics table.
How to File a Claim with an Indemnity Health Plan
Filing a claim under an indemnity health insurance plan is crucial since the policy reimburses your actual medical expenses. Following the proper steps ensures a smooth, timely settlement. Here’s a practical guide:
1) Inform the Insurer Promptly
- Emergency admission: Call, email, or use the insurer’s app/hospital network/ insurance desk within 24 hours of hospitalisation.
- Planned procedures: Submit a pre-authorisation request 48–72 hours prior to admission. Early intimation keeps your cashless option available and avoids delays. You can also inform your insurance intermediary for support.
2) Opt for a Network Hospital for Cashless Treatment
- Present your health card or policy number at the TPA desk.
- The hospital sends a pre-authorization request; the insurer must respond within the IRDAI-mandated three-hour window.
- Once approved, you pay only non-admissible charges and sign discharge documents.
- Some hospitals may ask for a refundable security deposit (₹5,000–₹50,000), which is common but not mandatory.
3) Reimbursement if Cashless is Not Available
- Pay all bills yourself and retain original receipts.
- Submit the completed claim form along with documents within 30 days of discharge (some insurers allow up to 60 days depending on circumstances).
- While insurers aim to settle claims within 15–30 days, real-world data shows that 2 in 5 reimbursement claims exceed 30 days, making cashless treatment preferable.
4) Keep a Complete Document Kit Ready
- Completed and signed claim form
- Photo ID (Aadhaar, PAN, Passport)
- Doctor’s admission note and prescriptions
- Final hospital bills, payment receipts, and discharge summary
- Pharmacy invoices, diagnostic reports, and investigation films
- Indoor Case Papers (ICP)
- FIR/police report or post-mortem (for accidents or death)
- Any additional documents requested by the insurer
Following these steps ensures your claim is processed quickly and accurately, helping you focus on recovery rather than paperwork.
Having said that, not all health insurance plans operate in the same manner. Broadly, they fall into two categories: Indemnity Policies, which cover actual medical expenses, and Fixed Benefit Policies, which pay a predetermined amount for specific events. Understanding the difference helps you choose the right coverage for your needs. The table below breaks down the key distinctions between the two.
Difference between an Indemnity Policy and a Fixed Benefit Policy
| Feature | Indemnity Health Insurance | Fixed Benefit Policy |
|---|---|---|
| Payout Type | Reimburses actual medical expenses incurred during hospitalisation, up to the sum insured. | Pays a fixed lump sum on the occurrence of a covered event (e.g., critical illness, accident). |
| Coverage Scope | Covers hospitalisation, surgery, room rent, ICU, medicines, pre- & post-hospitalisation, daycare, and sometimes OPD/maternity (depending on plan). | Covers specific events like diagnosis of listed illnesses, accidents, or hospitalization, irrespective of actual costs. |
| Example | Hospital bill is ₹2 lakh; sum insured ₹10 lakh → insurer pays ₹2 lakh, ₹8 lakh remains for future claims. | Critical illness plan with ₹10 lakh cover → diagnosed with cancer; insurer pays full ₹10 lakh, even if treatment costs ₹3 lakh. |
| Flexibility of Use | Money is used only for medical expenses. | Lump sum can be used for medical or non-medical purposes (travel, income loss, recovery help). |
| Premium Pattern | Premium depends on age, sum insured, and plan features; it generally rises with age and inflation. | Standalone fixed benefit premiums also rise with age, but term insurance-linked riders can be more cost-effective as their premiums are fixed for the rider duration. |
| Recommended For | Anyone seeking comprehensive hospitalisation coverage and protection against actual medical bills. | Supplementing indemnity plans for extra financial support during critical illness or accidents. |
Example: Indemnity vs Fixed Benefit
Indemnity Plan:
- Plan: HDFC ERGO Optima Secure (₹15 lakh cover)
- Scenario: You are hospitalized for dengue, and your hospital bill is ₹1.2 lakh.
- Outcome: The insurer reimburses ₹1.2 lakh, leaving ₹13.8 lakh of your sum insured for future claims. All actual medical expenses like room rent, ICU, and surgery charges are covered.
Fixed Benefit Plan:
- Plan: HDFC ERGO Critical Illness Platinum Care (₹10 lakh cover)
- Scenario: You are diagnosed with early-stage cancer. The treatment costs ₹3 lakh.
- Outcome: The insurer pays the full ₹10 lakh lump sum immediately, regardless of the actual hospital expenses. You can use this money for treatment, recovery, or even non-medical expenses like travel or income loss.
How to Find and Enrol in an Indemnity Plan? (Ditto’s Take)
An indemnity health insurance plan is non-negotiable — it’s the only way to protect yourself from unexpected out-of-pocket medical expenses. When hospitalisation occurs, it reimburses actual costs for room rent, surgery, ICU, medicines, and more.
Finding an indemnity plan is simple:
- Assess your needs – Consider your age, medical history, family size, and desired sum insured.
- Check the market – Compare leading plans and insurers.
- Evaluate key metrics – Look at Claim Settlement Ratio (CSR), Insurer Claim Ratio (ICR), complaint volume, insurer scale/solvency, and the network hospital strength of shortlisted insurers.
- Select a plan – Choose the one that fits your coverage needs, network convenience, and budget.
Fixed benefit plans are better as riders on term insurance. Standalone fixed benefit health plans have premiums that rise with age and often cover fewer illnesses. Term-linked riders, like Critical Illness or Accidental Total & Permanent Disability, provide broader protection and locked-in premiums for the policy term. Keep in mind, however, that fixed benefit riders with term plans may not be lifetime renewable and usually cap coverage at 20 years.
If you want to know which documents are required to apply for an indemnity health insurance plan, you can refer to this article.
Finding the best indemnity plan doesn’t have to be overwhelming. Our IRDAI-certified advisors can help you compare options, evaluate claims experience, and shortlist plans that match your needs — all for free. Book a call today and get personalised guidance without any pressure to buy.
Why Should You Approach Ditto for Your Health Insurance?
At Ditto, we’ve assisted over 7,00,000 customers with choosing the right insurance policy. Why customers like Abhinav below love us:
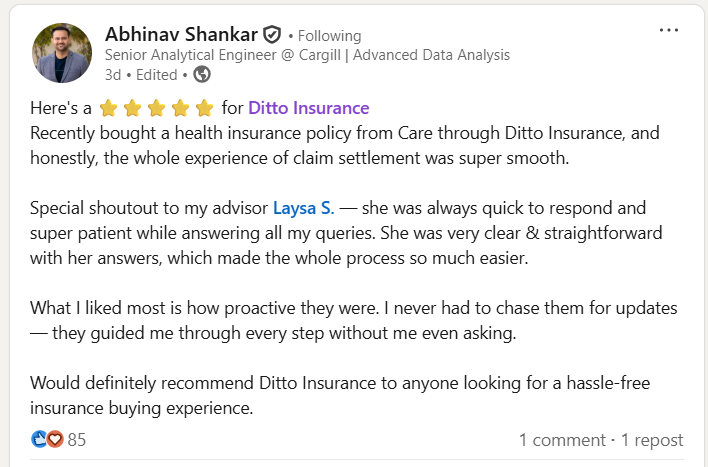
✅No-Spam & No Salesmen
✅Rated 4.9/5 on Google Reviews by 5,000+ happy customers
✅Backed by Zerodha
✅100% Free Consultation
You can book a FREE consultation. Slots are running out, so make sure you book a call now!
Conclusion
Indemnity health insurance is the foundation of financial protection against medical emergencies. By reimbursing actual hospitalisation costs, it ensures you are not burdened with out-of-pocket expenses for room rent, surgeries, ICU care, or pre- and post-hospitalisation costs.
While fixed benefit plans or riders can provide additional financial support, an indemnity plan is non-negotiable for anyone seeking comprehensive, reliable health coverage. Choosing the right plan involves assessing your needs, comparing insurers, and checking key metrics like CSR, ICR, and network hospital strength.
FAQs
Who should opt for Indemnity Health Insurance?
Anyone looking to cover actual hospitalisation expenses should opt for an indemnity plan. It is especially recommended for individuals with families, seniors, or those with potential future medical needs, as it prevents high out-of-pocket costs during hospital stays.
Can I combine an indemnity plan with a fixed benefit rider?
Yes. While indemnity plans cover actual medical bills, you can add a Critical Illness or Accidental Disability rider to provide extra financial support for specific events. Term insurance riders often have locked premiums for the policy term while health insurance rider premiums increase with age and inflation.
Are pre-existing diseases covered immediately?
No. Pre-existing conditions typically have a waiting period of 2 to 3 years, depending on the insurer. Coverage begins only after this period. Insurers do offer riders that can reduce these to day 1.
Is cashless hospitalisation guaranteed under an indemnity plan?
Cashless treatment is available at network hospitals, but you must notify the insurer promptly and follow the pre-authorisation process. Non-network treatments can be claimed via reimbursement.
Can I include maternity or OPD coverage in an indemnity plan?
Yes, but these are often optional add-ons or riders. Not all plans cover maternity or OPD by default.
How much sum insured should I choose?
Choose a sum insured based on family size, medical inflation, lifestyle, and expected hospitalisation costs. Higher coverage ensures financial security during major illnesses. However, a good rule of thumb is to get a minimum coverage of 10-15 lakhs for an individual or small family whereas larger families and people living in metro cities may require 20 to 30 lakhs of coverage. Also ensure that the plan has no limits on room-rent, no copay, no disease-wise sub-limits, offers consumables cover, a comprehensive bonus, and unlimited restoration.
Last updated on:










