What Is the Waiting Period for Kidney Stone Treatment in Health Insurance?
In India, kidney stone cases are rapidly increasing as a result of inadequate hydration and unhealthy eating patterns. According to several experts, cases have risen by 30–40% recently.
Worried about whether your health insurance covers kidney stones? You're not alone. Understanding waiting periods and the fine print of your policy can help you avoid unexpected medical expenses.
At Ditto, we've helped thousands navigate the complexities of kidney stone coverage, whether it's figuring out if it counts as a pre-existing condition or what happens if you're diagnosed after buying a policy. This article explains everything you need to know: waiting periods, if they can be reduced, and health insurance plans in India that offer kidney stone treatment.
Not sure about waiting period? Talk to Ditto’s expert advisors today and get unbiased, personalised guidance - absolutely free.
Did You Know?
What if Kidney Stones is a pre‑existing condition?
If you've previously been diagnosed with kidney stones, whether or not you've received treatment, most insurers will classify it as a Pre-Existing Disease (PED). And that comes with some important implications.
Let's break it down in plain terms:
- 30-Day Buffer Period: After After receiving treatment or being discharged from the hospital for kidney stones, there is typically a mandatory 30-day waiting period before you can apply for a new health insurance policy. During this period, most insurance providers will not accept a new application.
- Full Disclosure is Mandatory: Even if you're symptom-free or have used only alternative treatments (like Ayurveda or homeopathy), you must declare your kidney stone history when applying for insurance.
- Coverage is Conditional: having had Kidney stones doesn't automatically prevent you from getting health insurance. However, your eligibility and coverage can depend on a few factors, such as whether you need surgery, the size and location of the stone, and any related health issues, such as diabetes, high blood pressure, or frequent infections.
- Waiting Period of Up to 3 Years: Some health insurance plans will cover kidney stone-related treatments, but only after a waiting period of 2 to 3 years.
Did You Know?
Can the Waiting Period for Kidney Stone Treatment Be Reduced?
In most health insurance policies, kidney stones fall under a "specific illness" category, which carries a standard 2-year waiting period, regardless of whether the condition is newly diagnosed or pre-existing.
If you already have kidney stones before buying the policy, it will be treated as a pre-existing disease (PED). In this case, even if you opt for a PED buy-back rider to reduce or eliminate the PED waiting period, the 2-year waiting period for specific illnesses still applies.
Some plans, like Care Supreme or ICICI Elevate with their PED Waiting period reduction add-ons, reduce waiting periods for PEDs to as low as 1 year. For example, Aditya Birla Activ One Max allows you to reduce the PED waiting period to as low as 1 year with an add-on. However, these do not override the 2-year waiting period for specific illnesses like kidney stones.
Certain health insurance plans, such as Care Supreme or ICICI Elevate, offer add-ons that can reduce the waiting period for pre-existing diseases (PEDs) to as little as one year.
For instance, Aditya Birla Activ One Max lets you shorten the PED waiting period to one year with an add-on (Reduction in PED) . However, these add-ons do not bypass the standard two-year waiting period for specific conditions like kidney stones.
The implication? Buying an add-on solely to cover kidney stones early may not offer any real-time advantage, since the specific illness clause still applies independently.
Key Takeaway:
Buying an add-on to cover kidney stones early isn’t very useful, as the specific illness wait applies separately. Focus instead on reducing your pre-existing disease (PED) waiting period to 2 years (not 1) for more practical and broader health insurance benefits.
POINT TO BE NOTED
What if Kidney Stone is Diagnosed after Buying Health Insurance?
If you're diagnosed with kidney stones after you purchase a health plan, treatment is usually covered, but with certain conditions:
1) Most health insurers list kidney stones under "Specific Diseases," which often come with a 2-year waiting period, even if the condition wasn't pre-existing.
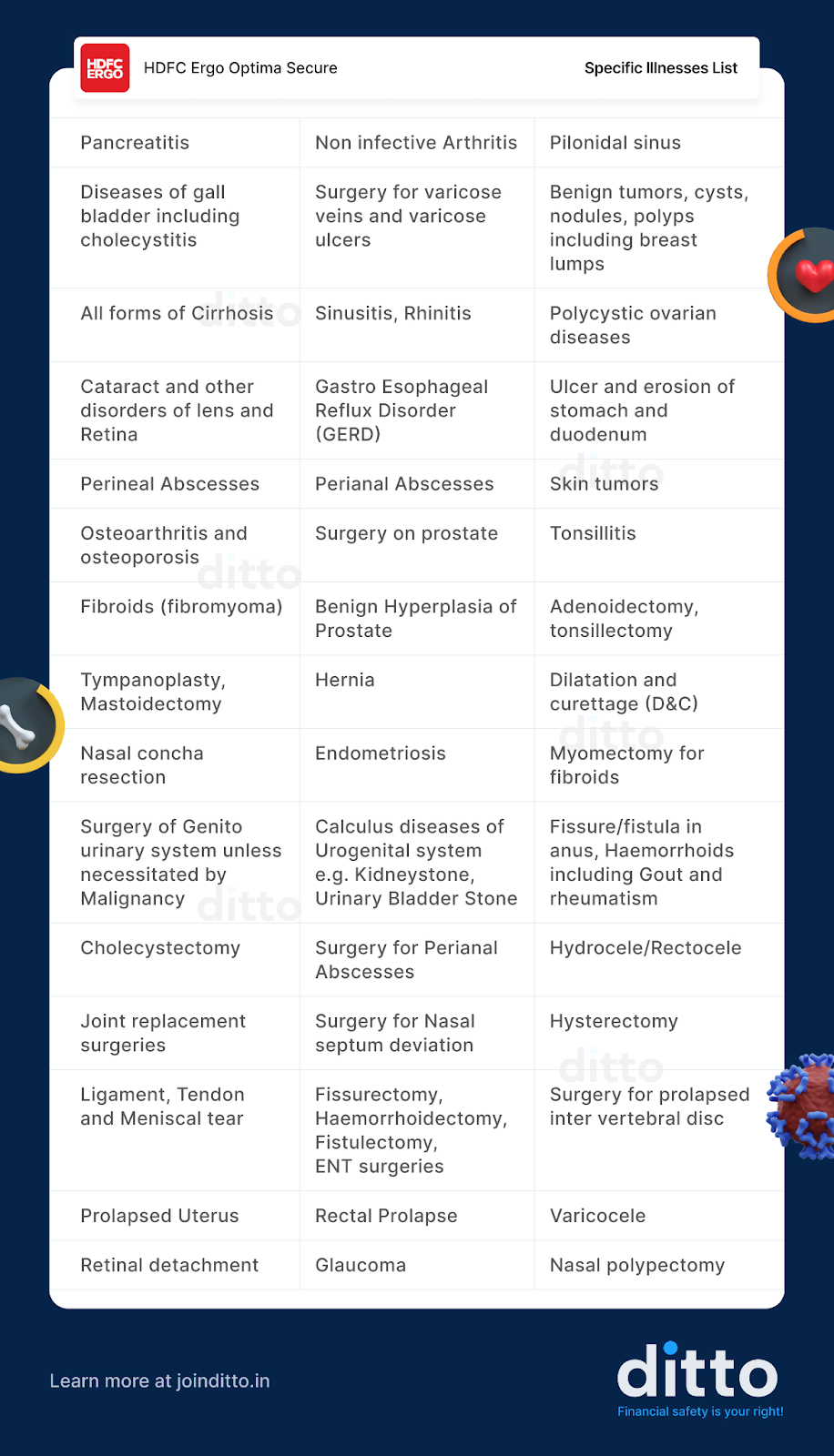
A standard 2 year waiting period, even if it’s a PED. Most “specific diseases” lists typically include other slow-developing conditions as well. Take, for example, a popular plan like HDFC Optima Secure:
2) OPD-only treatment, such as managing stones with medication and fluids, without hospitalisation, is not covered unless your policy includes OPD benefits or an OPD rider.
3) Daycare procedures like lithotripsy or ureteroscopy are covered if:
- The waiting period has been serve
- All documentation is in order
- Falls Under Daycare Treatment
Daycare treatment refers to:
In short, once the waiting period is over and documentation is proper, kidney stone removal procedures like lithotripsy qualify as daycare treatments and are covered.
So how do you pick a policy that actually covers kidney stones effectively?
Health Insurance Plans for Kidney Stones (That Make Ditto’s Cut
Most comprehensive insurance policies offer coverage if you have mild symptoms of kidney stones. If it is a PED, there’s no clear-cut path, and after proper underwriting, you are offered a plan with adequate coverage and a 2 to 3 year waiting period. As most plans cover Day care procedures like treatment of a Kidney stone, take a quick look at Ditto’s recommended health policy for kidney stone coverage:
Why Choose Ditto for Health Insurance?
At Ditto, we’ve assisted over 8,00,000 customers with choosing the right insurance policy. Why customers like Abhinav below love us:

- No-Spam & No Salesmen
- Rated 4.9/5 on Google Reviews by 15,000+ happy customers
- Backed by Zerodha
- 100% Free Consultation
You can book a FREE consultation. Slots are running out, so make sure you book a call now!
Kidney Stone Waiting Period in Health Insurance: Ditto’s Take
According to experts at Ditto, complete transparency is crucial when buying health insurance. Even if you’ve only had mild kidney stone symptoms, taken Ayurvedic remedies, or experienced a minor episode years ago, you must disclose it. Failing to do so, even if the condition is treated can lead to claim rejection or policy cancellation later.
Corporate health plans usually cover kidney stone treatment from day one, while personal plans at least have a 2-year waiting period. When purchasing a policy, review sub-limits, exclusions, and pre-authorization rules to avoid unexpected claim rejections.
Conclusion
Kidney stone coverage isn’t optional—it’s essential. Most health insurance plans include treatment, including daycare procedures like lithotripsy and ureteroscopy. However, if you’ve had symptoms or treatment before buying the policy, a 2-year waiting period will be applied.
To ensure hassle-free claims, buy insurance early and always disclose your complete health history—even mild or past episodes. Look for plans that cover day care treatments, have flexible terms, and clearly outline waiting periods.
Not sure which one to pick? Book a free call with Ditto’s advisors to find a policy that fits your needs.
FAQs
Is a kidney stone a pre-existing condition?
Yes. If you've had any symptoms, diagnosis, or treatment (including Ayurvedic or homeopathic) before buying your policy, it's considered a pre-existing disease (PED). It becomes essential to declare it during policy purchase since the insurer classifies a condition as PED only if its disclosed.
What treatments are covered?
Most health plans cover procedures like lithotripsy, ureteroscopy (URSL), PCNL, and hospitalisation for complications—but only after waiting.
Is hospitalisation for pain covered?
Yes, if you're admitted for acute pain due to kidney stones, and the waiting period is complete, expenses are typically covered.
What if treatment is non-surgical?
Outpatient (OPD) treatments like medication or fluids are only covered if your policy includes OPD benefits.
Will a Corporate Health Plan Cover Kidney Stone Treatment?
Yes, most corporate plans cover kidney stone treatment, including hospitalization and surgery, without a waiting period.
Last updated on: